General information:
Before we explain “Chiari malformation”, we would like to explain the area of the body in which a Chiari malformation presents itself: In a normal development of the skull and brain, everything is in its place and fulfills its function there. The cerebrum and cerebellum are arranged in such a way that they have a fixed position in the skull and are not impaired or restricted by the skull bones.

Illustration: Normal skull with normal organ arrangements
The spinal cord originates in the brain and extends in the spinal canal up to the first/second lumbar vertebra. The spinal column provides a protective sheath for the spinal cord.
Nerve fluid (cerebrospinal fluid) is constantly produced in the ventricles of the brain, then flows through the ventricular system and washes around the brain.
At the end of the cerebellum, it is released through the posterior cranial fossa into the spinal canal, where it pulsates rhythmically and flows around the spinal cord.
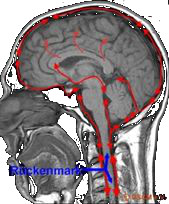
Illustration: Circulation of cerebrospinal fluid in the skull and spinal canal.
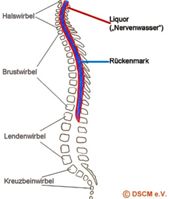
Figure: Schematic representation of the spinal column with spinal cord and cerebrospinal fluid.
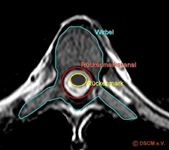
Illustration: Horizontal cross-section through a thoracic vertebra with drawing of the spinal cord and spinal canal.
In the middle of the spinal cord is a central canal that is surrounded by gray matter, i.e. a cord of nerve tissue. The gray matter is embedded in white matter and covered by various membranes (soft meninges, spider web membranes and hard meninges). Various nerves (spinal nerves) originate from the spinal cord and transmit motor signals from the brain via peripheral nerves to the skin, bones, muscles and joints (in the same way as they transmit sensory information to the brain). Each nerve supplies a limited area of skin and a specific muscle group; thoracic nerves largely supply the skin and muscles of the trunk, whereas the anterior branches of the cervical, lumbar and sacral nerves form complex plexuses.
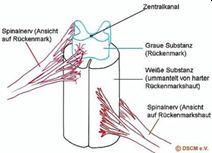
Figure: Spinal nerves emanating from the spinal cord (depending on the level of exit, eight cervical nerves, twelve thoracic nerves, five lumbar nerves, five sacral nerves, and one stone nerve.
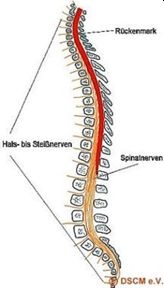
Figure: Schematic representation of the spinal cord with an exemplary, simplified drawing of the spinal nerves. Spinal nerves always emerge from the spinal cord in pairs (four spinal nerves should therefore be shown here).
What is Chiari malformation?
Chiari malformation (formerly known as Arnold-Chiari malformation or ACM for short) is one of the most common embryonic developmental disorders, 8 per 100,000, and develops in the 6th-10th week of pregnancy.
Chiari malformation is a bony malformation of the cranial margin and the first cervical vertebrae. These bony changes mean that there is not enough space under the skull for some of the posterior parts of the brain (cerebellum, cerebellar tonsils). Due to this lack of space, they look for a new place and this is then the transition between the skull and the spinal column. The displaced parts of the brain protrude through the occipital foramen into the spinal canal or outwards. Due to the different manifestations, Chiari malformation is divided into types I, II, III and IV.
Type I is characterized by a displacement of the cerebellar tonsils, usually accompanied by syringomyelia (i.e. a constantly changing cavity formation in the spinal cord, see there).
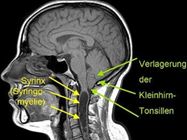
Figure: Chiari malformation type I (marked by green arrows), here additionally with a syrinx (cavity in the spinal cord), i.e. a syringomyelia.
Occasionally, bony malformations of skull bones and vertebrae can also be diagnosed in Chiari malformation type I. This form of Chiari malformation is usually fully developed by the second or third year of life, although the health complaints are often not clearly noticeable until around the age of thirty.
Type II is characterized by a slight to severe displacement of the cerebellum combined with a malformation of the brain stem.

Figure: Displacement of cerebellar tonsils, cerebellar vermis and brain stem into the spinal canal with enlargement of the large occipital foramen (not shown).
In addition, nerve cells die in the displaced brain tissue. In around 80 % of those affected by Chiari malformation type II, the ventricles of the brain, which form the cerebrospinal fluid, are abnormally altered, resulting in a build-up of cerebrospinal fluid, which causes the skull to grow in volume – this is known as hydrocephalus (also known colloquially as hydrocephalus).
Type III, which is largely identical to type II except for the complete displacement of the cerebellum and/or brain stem to the neck, is rare. This tissue displacement can occur if there is a gap in the skull bone, which is known as an encephalocele.
Even rarer is type IV, which describes a genetically caused underdevelopment (hypoplasia) of the cerebellum with a smaller posterior fossa, which is essentially filled with cerebrospinal fluid.
Causes:
As a rule, a Chiari malformation is congenital and therefore a malformation in the growth phases of the fetus. Chiari malformation is not inherited.
In rare cases, a Chiari malformation is acquired, for example when a brain tumor or a severe birth injury pushes the cerebellum into the spinal canal.
Symptoms and course:
The symptoms depend on the type of Chiari malformation and whether there are additional diseases such as syringomyelia or spina bifida (open back).
Otherwise, the symptoms can be outlined as follows:
– Head and neck pain
– Compression syndrome
– Flaccid paralysis, incomplete paralysis of the arms and legs
– Sensory disorders, sensory deficits, coordination disorders
– Rolling and twisting of the eyes (nystagmus)
– Speech disorders
– Decreased swallowing reflex with difficulty swallowing
– Difficulty breathing and even swallowing liquids
– Whistling breathing sounds when the upper airways are constricted or displaced
– Hyperextension of the trunk, arms and legs
Diagnosis:
The diagnosis of a Chiari malformation is made with the aid of computer tomography or, for more detailed imaging, with the aid of magnetic resonance imaging (MRI, also known as magnetic resonance imaging), an imaging procedure that does not use X-rays. The images of the skull, brain and spinal canal clearly show the changes characteristic of Chiari malformation in both the skull and brain.
Secondary findings, such as the existence of a syrinx, can also be determined in terms of location and extent. Other pathological changes such as tumors can be made visible by using a contrast agent that is injected during the examination.
In order to visualize the circulation of the cerebrospinal fluid in the skull or in the spinal canal, specialized clinics are able to record the flow using a special MRI examination. The pulsation of the cerebrospinal fluid is displayed in relation to the heartbeat of the person being examined. Experienced and precise analysis of the image of the cerebrospinal fluid flow obtained in this way allows even the smallest adhesions with impaired circulation of the cerebrospinal fluid to be detected.
The removal of cerebrospinal fluid from the spinal canal (lumbar puncture) can provide important indications of other pathological changes in the central nervous system, but should only be carried out after a prior examination of the head using computer tomography or magnetic resonance imaging in order to obtain clear findings on the intracranial pressure conditions before the cerebrospinal fluid is removed.
In fetuses, prenatal diagnostic sonography procedures are available to diagnose Chiari malformation.
Therapy:
The aim of any treatment for Chiari malformation is to eliminate the malformation and its effects.
In type I, this is done by an operation in which the large occipital foramen is widened and any bony malformations of the skull are corrected. Any syringomyelia often regresses as a result.
In type II, a drain is first surgically created for the accumulated cerebrospinal fluid and otherwise the procedure is the same as for type I.
In types III and IV, viability and operability depend very much on the circumstances of the individual case, so that no statements can be made about treatment here.
In all cases, however, diagnosis and treatment should be carried out by highly experienced neurosurgeons.
Mila & Paul (German)
The disease