General information:
Before we explain “syringomyelia”, we would like to explain the area of the body in which syringomyelia presents itself: Our spine provides a protective sheath for the spinal cord. The spinal cord originates in the brain and extends in the spinal canal up to the first/second lumbar vertebra. It measures up to 45 cm in length.
Nerve fluid (cerebrospinal fluid) is constantly produced in the ventricles of the brain, then flows through the ventricular system and washes around the brain. At the end of the cerebellum, it is released through the posterior cranial fossa into the spinal canal in a rhythmic, pulsating manner, where it washes around the spinal cord.
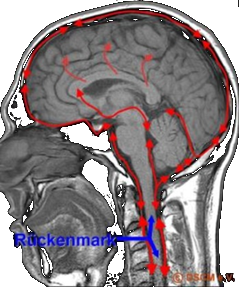
Illustration: Circulation of cerebrospinal fluid in the skull and spinal canal

Illustration: Schematic representation of the spinal column with spinal cord and cerebrospinal fluid
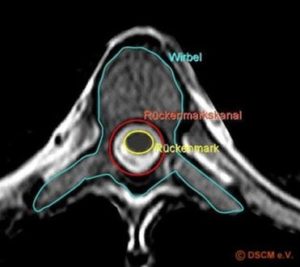
Illustration: Horizontal cross-section through a thoracic vertebra with drawing of the spinal cord and spinal canal
In the middle of the spinal cord is a central canal surrounded by gray matter, i.e. a cord of nerve tissue. The gray matter is embedded in white matter and covered by various membranes (soft meninges, spider tissue membranes and hard meninges). Various nerves (spinal nerves) originate from the spinal cord and transmit motor signals from the brain via peripheral nerves to the skin, bones, muscles and joints (in the same way as they transmit sensory information to the brain). Each nerve supplies a limited area of skin and a specific muscle group; thoracic nerves largely supply the skin and muscles of the trunk, whereas the anterior branches of the cervical, lumbar and sacral nerves
form complex networks called plexuses.

Illustration: Spinal nerves emanating from the spinal cord (eight cervical nerves, twelve thoracic nerves, five lumbar nerves, five sacral nerves and one coccygeal nerve, depending on the level of exit).
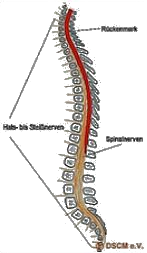
Illustration: Schematic representation of the spinal cord with an exemplary, simplified drawing of the spinal nerves. Spinal nerves (five spinal nerves should therefore be shown here).
What is syringomyelia?
In syringomyelia, a rare disease in the spinal canal, the gray matter of the spinal cord contains a mostly elongated, fluid-filled cavity (the syrinx), which displaces the gray matter and contains no nerve cells. Several or even just one syrinx can form, particularly in the spinal cord area of the cervical and thoracic spine.
This may be associated with, but in any case causes, an impairment or even severe obstruction of the circulation of the cerebrospinal fluid.
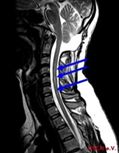
Illustration: Syrinx in the middle cervical and thoracic vertebrae, marked by arrows

Illustration: Long, narrow syrinx from the neck to the lumbar region, marked by arrows
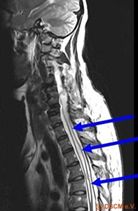
Illustration: Horizontal cross-section through a thoracic vertebra with drawing of the spinal cord and canal.
There is no correlation between the size of a syrinx or the number of syringomyelia and the severity of the disease, just as there is usually no causal relationship between the location of the syrinx and symptoms. Once formed, the syrinx can grow in size over the years. However, not every syrinx is a syringomyelia, so there are also syrinx formations that do not expand further until the end of life and are strictly speaking not a syringomyelia but a hydromyelia.
Contrary to outdated doctrine, syringomyelia is not a disease of the soul/psyche and has nothing to do with a mental illness!
Causes:
As already mentioned, the syrinx that has formed in the spinal cord displaces nerve tissue, which is known as syringomyelia. But how does syringomyelia develop?
First of all, a distinction is made between congenital and acquired syringomyelia – what both have in common is the formation of a cavity in the spinal cord and the fact that the cerebrospinal fluid cannot circulate freely. In syringomyelia, the syrinx is filled with cerebrospinal fluid.
The causes of acquired syringomyelia have not yet been conclusively determined scientifically. What is certain, however, is that the cause of acquired syringomyelia is always an obstruction of the cerebrospinal fluid circulation: If the circulation of the cerebrospinal fluid in the spinal canal is blocked at one point, the cerebrospinal fluid seeks another route in the narrowness of the spinal canal and a syrinx develops.
There are many reasons that can lead to a blockage of the cerebrospinal fluid circulation. They can be malformations or inflammations that cause adhesions of the fine spinal cord membranes (spinal meninges). Accidents, tumors and severe herniated discs can also be the reason for the blockage and development of a syrinx, although the syrinx does not have to occur at the exact site of the injury.
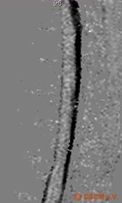
Illustration: Normal, undisturbed cerebrospinal fluid circulation (black)
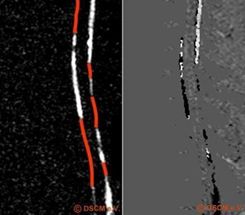
Illustration: Disturbed circulation of cerebrospinal fluid.
In the left image, the lack of circulation is shown in red. The image on the right shows the same nerve water circulation disorder as it originally appears in the MRI.
Words and definitions that are also used in connection with syringomyelia should also be mentioned here: The terms hydromyelia and syringomyelia are often used as if they both have the same meaning. However, hydromyelia refers to an enlargement of the central canal that is congenital and non-progressive. However, the differences are very fluid.
Syringobulbia (also known as syringoencephalomyelia) is the term used when the congenital cavity extends into the lower sections of the brain. Syringoencephaly is in turn a cavity formation in the brain.
Symptoms and progress:
The symptoms of syringomyelia are very varied and can be related to the location of the syrinx in the spinal cord. We must therefore expressly point out that the following list of typical symptoms does not necessarily apply to every patient, nor does it necessarily apply in full.
Typical complaints may include the following (in no particular order and without any claim to completeness):
- Severe sharp, burning or dull pain in the shoulder, head, neck and arm areas, migraine-like headaches
- Sensitivity disorders such as insensitivity to heat in individual parts of the skin of the limbs; sensitivity to touch in the limbs; disturbance of depth sensitivity
which indicates the position of the body or limbs); increased sensitivity to heat or cold - Disorders of the sense of position, gait instability, dizziness and coordination disorders, temporary memory disorders
- Sensory disturbances in the limbs such as tingling or stinging
- Cramps (e.g. muscle spasms), uncontrolled muscle twitching (fasciculations), signs of paralysis or paralysis, reduction in muscle mass
(muscle atrophy) - Incontinence of the bladder and bowel up to paralysis of the bladder or sphincter muscle
- Perceptual disorders in vision and hearing, sensory disorders, speech disorders
- Impotence, decreasing libido, sexual dysfunction
- Dysregulation-related circulatory disorders; slower wound healing
- Difficulty swallowing, tongue dysfunction
- States of fatigue, general weakness, tendency to rapid exhaustion
- Insomnia, depressive mood (up to and including depression)
Diseases associated with the syrinx can be malformations, inflammations, tumors and hydrocephalus in the head area. In the area of the spine, malformations, inflammation, tumors, wear and tear (degeneration) and, as mentioned above, adhesions.
Diagnosis:
A syrinx is diagnosed exclusively with the help of magnetic resonance imaging (MRI, also known as magnetic resonance imaging), an imaging procedure that does not use X-rays. The position and extent of the syrinx can be clearly visualized in the images of the spinal canal and the adjacent parts of the brain. The examination is always carried out with contrast medium during the initial diagnosis and covers the entire nervous system.
In order to visualize the circulation of the cerebrospinal fluid in the skull or in the spinal canal, specialized clinics are able to record the flow using a special MRI examination. The pulsation of the cerebrospinal fluid is displayed in relation to the heartbeat of the person being examined. Experienced and precise analysis of the image of the cerebrospinal fluid flow obtained in this way allows even the smallest adhesions with impaired circulation of the cerebrospinal fluid to be detected.
Finally, an examination of the cerebrospinal fluid should always be carried out in order to rule out any inflammation. For this purpose, the cerebrospinal fluid is taken by means of a so-called lumbar puncture, a painless puncture in the lumbar vertebrae using a specially sharpened needle.
The use of myelography (or post-myelo-CT), in which the nerve fluid space is punctured in the lower lumbar spine and enriched with contrast medium in order to determine the extent of the inflammation, is rather uncommon today.
Therapy:
It is currently not possible to cure a syringomyelia. Furthermore, it does not make sense to treat the syrinx, but for the time being the cause of the syrinx must be eliminated as far as possible.
It is important that the patient learns to recognize and respect their body and its signals.
Nevertheless, the following treatment options are available:
1. surgically:
There are various ways of surgically influencing the syrinx so that it collapses or decompresses. The aim is to significantly reduce the pressure that the syrinx exerts on the tissue and thus positively influence the progression of the disease.
To this end, a drainage option (shunt) for the syrinx can be created, for example by means of a tube that is placed depending on the position of the syrinx and allows the fluid in the syrinx to drain into the abdominal cavity, for example (syringoperitoneal shunt). Nowadays, the placement of a shunt is no longer favored. It is also possible to create a drainage option without a tube (so-called marsupialization).
A shunt should only be inserted if there is no other treatment option. Pain can be reduced in this way, but damage that has already occurred (motor or sensory) cannot usually be reversed.
In any case, such an intervention should only be carried out by specialized neurosurgeons after thorough examination and consultation. After all, every time a shunt is inserted, tissue is damaged and a foreign body remains in the spinal cord/spinal canal, so careful consideration is required. The sustainability of the procedure varies greatly and also depends on the type of shunt. The closure rate of such shunts is up to 80 %.
It is much better to avoid adhesions in the spinal canal, which can lead to circula
Mila & Paul (German)
The disease